So You Want To Be A Pathologist?
Think back to the last time you visited a clinic or hospital with a problem. How many people were involved with diagnosing and treating you? If you said one, you’d be like the many others who refer to a clinical physician as their sole healthcare provider. However, you’d also be incorrect; they are NOT doing all of that work alone! Instead, pathologists do the behind-the-scenes work required for them to swoop in and save the day. Routine things seen everyday such as blood or urine tests, searches for infection, and allergy diagnoses all involve pathologists!
Generally, pathology is the study of disease and illnesses, and is often called “the basis of all clinical medicine.” The field bridges the gap between science and medicine to introduce things like laboratory applications to diagnostic testing and innovative genetic technologies to disease prevention. If the science behind medicine is more interesting to you than the aspect of direct patient-care, pathology may be an excellent choice for you to consider. In this inaugural “So You Want To Be” series post, we will explore what a pathologist is, the many different types of pathologists, the post-medical graduate programs that allow you to pursue a career in the field, and the pros and cons of choosing to become a pathologist.

What is a Pathologist?
A pathologist is a highly-specialized physician who has the primary role of examining and interpreting parts of our bodies using laboratory tests. This is done to understand the causes, characteristics, and effects of diseases as these provide essential information for other types of physicians that will help them confirm diagnoses of illnesses, monitor ongoing medical conditions, and help guide patient treatment. These parts of our bodies include surgically-removed organs; tissues from biopsy samples; and bodily fluids such as urine, mucus, and blood. For example, an anatomical pathologist may examine a patient’s kidney tissues using a microscope to determine if the patient is in need of a transplant. If so, the pathologist would communicate the information to the patient’s physician or surgeon accordingly. Seeing that pathologists use collected information to help other physicians understand and diagnose patient diseases, they make up a critical component of the medical community. And since pathology is such a massive field, the places pathologists work differ greatly, ranging from hospitals and laboratories to offices and classrooms.
Aside from examining and interpreting bodily specimens, individuals in this profession usually must also oversee the management of hospital/clinical labs, communicate with physicians to guide the diagnosing process and proper medical treatment for patients, conduct their own research, and present scientific findings. For example, check out this video where you can watch a webinar from the Ontario Association of Pathologists! The webinar is delivered by two speakers from Ontario’s very own William Osler Health System and discusses how the treatment of patients presenting with non-small-cell lung carcinoma (NSCLC) has changed in terms of biomarker testing, as well as how access to the treatment and testing of NSCLC should be maintained.

Types of Pathologists:
When reading the information about a pathologist’s responsibilities, it is important to understand that the roles of a pathologist vary depending on the type. These physicians are highly-specialized and enter into different branches of the field. Generally, Pathology/Laboratory Medicine is separated into five recognized medical specialties, Anatomical Pathology, General Pathology, Neuropathology, Hematological Pathology, and Medical Microbiology; one subspecialty (considering relevance to pathology), Forensic Pathology; and two Areas of Focused Competence, Transfusion Medicine and Cytopathology.
Before getting into the types of pathologists, however, an understanding of the medical-specialty system is important. There are 3 forms of specializations in Canada: Specialties, Subspecialities, and Areas of Focused Competence. Firstly, a Medical Specialty is a broad-knowledged branch of medicine that serves as the basis for additional training such as subspecialties and AFCs. Examples of these areas include General Surgery, Psychiatry, Emergency Medicine, etc. Next, a Medical Subspecialty is a branch of medicine that provides more focused/advanced training which is built upon the broad-knowledged parent specialty. For example, a subspeciality of Internal Medicine (a medical specialty) could be Cardiology. Finally an Area of Focused Competence is a branch of specialty medicine similar to a Fellowship that is meant to fulfill a public health need that is not met by the previously-established specialties and subspecialities. These further develop a physician’s certifications through extra/advanced training. Examples of AFCs are Hyperbaric Medicine, Trauma General Surgery, Sport and Exercise Medicine, and Sleep Disorder Medicine. The reason that physicians choose to further their training is to maintain their status as a competitive applicant and/or to expand their medical knowledge in areas that interest them.

Anatomical Pathology:
Anatomical Pathology is the medical specialty that deals with the study of morphologic (structure and form) and molecular aspects of disease, rather than their function. These pathologists are responsible for examining tissues to investigate and diagnose disease, collecting and interpreting information at both the macroscopic and microscopic level, and applying their judgement, knowledge, and skills to inform and/or guide the clinical decisions of other physicians. This aspect of assisting other physicians with a patient’s diagnosis is what makes the field of pathology so crucial to patient care! One great thing about Anatomic Pathology, however, is that these pathologists are not limited to seeing/doing the same thing everyday. The studying of tissue can range from looking at individual cells from a mass’ fine needle aspiration all the way to the evaluation of the entire body during an autopsy! Anatomical pathologists also have the privilege to study all organ systems in the human body including cardiovascular, dermal, endocrine, gastrointestinal, genitourinary, hematopoietic, neural and muscular, etc. and use interesting laboratory techniques such immunohistochemistry, flow cytometry, and electron microscopy to do their jobs! Interestingly, they also have the responsibility of providing summaries of clinical events leading to death by performing autopsies in complex medical cases along with cases of sudden/unexpected death.
To become certified in the medical specialty of Anatomical Pathology, a five-year accredited residency program must be pursued upon completion of medical school. In Ontario, there are five of these residency programs which are offered by the following institutions: The University of Toronto, McMaster University, Western University, Queen’s University, and the University of Ottawa. To get an idea of what an Anatomical Pathology residency program is like, we will explore the University of Toronto’s.
University of Toronto Anatomical Pathology Residency Program (program website)
- This is a five-year program operating under the department of Laboratory Medicine and Pathobiology. Individuals who are medical students or graduates who have obtained, or are in the process of obtaining, a medical degree from an accredited medical school can apply by July 1 of the match year through CaRMS
- Like most residency programs for pathology, this is exceedingly competitive and has a very low enrolment quota of approximately 2 people
- Residents will take part in core training that makes up the competencies of Anatomical Pathology such as general surgical pathology, cytopathology, pediatric and perinatal pathology, autopsy pathology, forensic pathology, molecular pathology, quality assurance, and principles of lab management. This will take place at major teaching hospitals and institutions such as Toronto General Hospital, Sunnybrook Health Sciences Centre, St. Michael’s Hospital, and more. For more insight, read this story of a previous resident where he explains his experience in the program and gives advice to others thinking of applying

General Pathology:
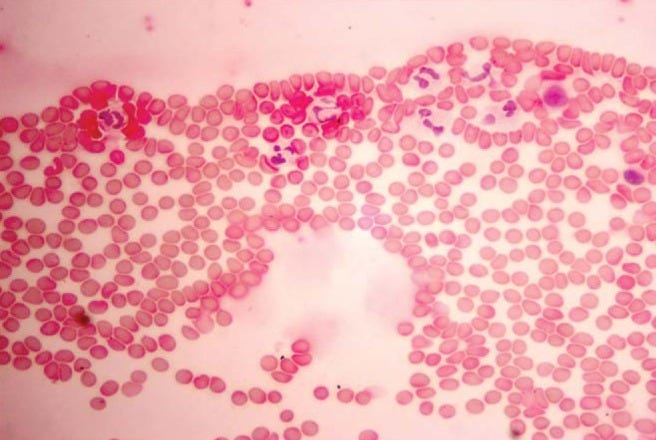
General Pathology is the medical specialty that focuses on the use of laboratory equipment to investigate and determine patient health and disease. It’s kind of an “all-in-one” pathology specialty since it includes areas falling under anatomical pathology such as surgical pathology, cytopathology, and forensic pathology, and areas falling under clinical pathology such as microbiology, biochemistry, hematological pathology, and transfusion medicine. General pathologists are responsible for guiding clinical decisions that only rely on laboratory tests to determine a disease’s presence, extent, and absence, and/or monitor the effectiveness of its treatments. They do this by examining samples of (usually) bodily fluid using a microscope or other diagnostic tools and reviewing its levels of particular substances. General pathologists then interpret this information and make a diagnosis or decision to do further study which is communicated to clinical staff. Laboratory tests like these can be as routine as testing for glucose and sodium and, at the same time, as uncommon as doing molecular testing for cancer markers and genome sequencing. Since these responsibilities involve General Pathologists in the day-to-day communications between clinical staff and the laboratory, they are often called the “bridge” between the two groups. In addition to working with many different types of physicians, General Pathologists also have the responsibility of overseeing the medical aspects of lab activity which includes the directing of laboratory quality assurance, utilization, and management.
To become certified in the medical specialty of General Pathology, a five-year accredited residency program must be pursued upon completion of medical school. In Ontario, there is only one, and it is offered by McMaster University.
McMaster University General Pathology Residency Program (program website)
- This is a five-year program operating under the department of Pathology and Molecular Medicine. Individuals who are medical students or graduates who have obtained, or are in the process of obtaining, a medical degree from an accredited medical school can apply by July 1 of the match year through CaRMS
- This is a very competitive program with an enrolment quota of approximately 1 person
- Residents spend the first year completing clinical rotations relevant to their program which exposes them to common pathology procedures including pathology specimens, bone marrow and fine needle aspirate
- In years two to four, residents complete a minimum of 36 block rotations in Anatomical Pathology and its related fields such as Cytopathology, Forensic Pathology, Hematological Pathology, Medical Microbiology, and Medical Biochemistry. This provides them with both anatomical and clinical knowledge which form the specialty of General Pathology
- In year five, residents are given the opportunity to take on more responsibility by doing full daily workload cases and working independently during calls in all branches of pathology, to develop and implement plans in quality assurance, and to continue their professional development through electives

Neuropathology:
Neuropathology is the heavily research-oriented medical specialty that focuses on the studying of primary and secondary diseases of the body’s central (brain/spinal cord) and peripheral nervous systems as well as its skeletal muscle. Although Neuropathologists, like Anatomical Pathologists, are responsible for examining bodily tissue, their branch of pathology requires them to focus solely on tissue of the nervous system, which they are extensively trained in. This aspect of focusing on only the nervous system allows them to work closely with neurologists and neurosurgeons. Continuing, these pathologists use a variety of laboratory techniques to examine biopsied nervous tissue which allows them to diagnose tumors, inflammatory disorders, and infections, therefore helping guide how clinical physicians should proceed with patient care. Along with biopsied tissue, Neuropathologists are also largely responsible for autopsied nervous tissue analysis. In this subsection, they often examine brain tissue to study dementia and genetic conditions, as well as to establish causes of death. Pursuing this further, neuropathology is, as mentioned, a heavily-research oriented field since these pathologists are increasingly becoming part of research teams that study diseases such as Alzheimer’s disease, Huntington’s Disease, and Parkinson’s disease through post-mortem tissue analysis. To catch a glimpse of what these neuropathologists do, take a look at this video to see a one carry out the diagnostic assessment of an autopsied brain!
To become certified in the medical specialty of Neuropathology, a five-year accredited residency program must be pursued upon completion of medical school. In Ontario, there are two of these residency programs which are offered by The University of Toronto and Western University. To get an idea of what a Neuropathology residency program is like, we will explore Western University’s.
Western University Neuropathology Residency Program (program website)
- This is a five-year program operating under the department of Pathology and Laboratory Medicine. Individuals who are medical students or graduates who have obtained, or are in the process of obtaining, a medical degree from an accredited medical school can apply by July 1 of the match year through CaRMS
- This residency program is particularly competitive and has a very low enrolment quota of approximately 1 person
- Residents spend the first year building a foundation of knowledge to prepare for the rest of the program and the second year studying Anatomical Pathology with subspecialty rotations in Neuropathology-related fields such as head and neck. ophthalmic, bone, and soft tissue pathology
- Third-year residents begin learning how to prepare, study, diagnose, and report on surgical (biopsied) and autopsy (post-mortem) tissue samples and more. They also gain exposure to disease patterns, neurocytology, pediatric neuropathology, forensic neuropathology and neuromuscular pathology
- Residents spend years four and five building on what was learned in year three and participating in added electives that suit intended career paths
Hematological Pathology:
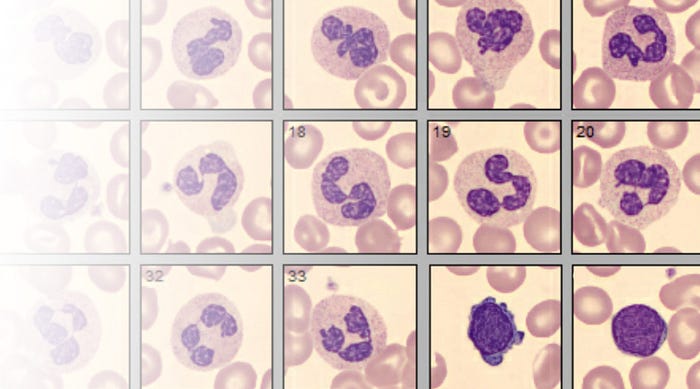
Hematological Pathology is the medical specialty relating to the use of laboratory equipment to study, investigate, diagnose, and therapeutically monitor blood disorders, blood-forming elements, hemostasis, and the immune function of adults and children. Hematological Pathologists have the responsibility of guiding physicians on how to proceed with patient care through evaluating and interpreting disorders of the blood cells, bone marrow, lymph nodes, the spleen, and hemostasis. For example, if a twenty-year old patient presents with a form of blood disease, a hematological pathologist would conduct specialized tests such as flow cytometry and/or immunohistochemistry with the affected sample, interpret the results, and communicate with the patient’s physician to discuss how they should treat them. Additionally, it is reported that these pathologists may also have the responsibility of organizing and running a transfusion medicine service as well as managing laboratory issues of blood and blood product procurement. As will be discussed below, transfusion medicine is a medical Area of Focused Competence involving the use of blood or blood products to prevent disease.
To become certified in the medical specialty of Hematological Pathology, a four-year accredited residency program must be pursued upon completion of medical school. In Ontario, there is only one of these residency programs that is accredited which is offered by The University of Toronto.
University of Toronto Hematological Pathology Residency Program (program website)
- This is a four-year program operating under the department of Laboratory Medicine and Pathobiology. Individuals who are medical students or graduates who have obtained, or are in the process of obtaining, a medical degree from an accredited medical school can apply by July 1 of the match year through CaRMS
- This residency program is particularly competitive and has a very low enrolment quota of approximately 1 person
- Like most programs, residents spend the first year building a foundation of knowledge to prepare for the rest of the program. They will spend years two to four in core hematology laboratory training with rotations in pediatric hematology, morphological evaluation of blood films, investigation of thrombosis and hemostatic disorders, laboratory management, and more! They are also encouraged to undertake a research project throughout their training

Medical Microbiology:
Medical Microbiology is a medical specialty that deals with bridging the areas of laboratory science and clinical medicine to diagnose, treat, and explore the prevention of infectious diseases, ultimately guiding the clinical decisions of other physicians and improving patient care. This type of pathologist is responsible for overseeing this diagnosis-treatment-prevention process of illnesses caused by microorganisms like viruses, fungi, and parasites. Medical Microbiologists do this by first providing their expertise on how and where to collect an appropriate sample that will diagnose an infection, including swabs — a method we now see as quite common with the testing procedures for COVID-19 — and tests for bodily fluids such as blood or urine. Then, they work with other microbiologists in hospital or outpatient clinic laboratories to examine the sample, discover the causes of infection, identify the best course of treatment for that particular infectious disease, and monitor patients throughout their recovery. Through this aspect of patient monitoring, Medical Microbiologists are also responsible for ensuring that antibiotic medications are prescribed and used appropriately to control the disease’s resistance to antimicrobial substances and, therefore, its spread. When asked about what she loves about her job, Dr. Larissa Matuka who is the Division Head of Microbiology at St. Michael’s Hospital, says, “What I love about my job is, really, the diversity in its scope of practice. Everyday there are new challenges and everyday there are different challenges; there’s never any two things that are alike.”
To become certified in the medical specialty of Medical Microbiology, a five-year accredited residency program must be pursued upon completion of medical school. In Ontario, there are three of these residency programs which are offered by the University of Toronto, the University of Ottawa, and McMaster University. To get an idea of what a Medical Microbiology residency program is like, we will explore the University of Ottawa’s.
The University of Ottawa Medical Microbiology Residency Program (program website)
- This is a five-year program operating under the department of Pathology and Laboratory Medicine. Individuals who are medical students or graduates who have obtained, or are in the process of obtaining, a medical degree from an accredited medical school can apply by July 1 of the match year through CaRMS
- This residency program is particularly competitive and has a very low enrolment quota of approximately 1 person
- Residents spend the first year building a foundation of knowledge to prepare for the rest of the program. This is done through rotations in areas such as General Internal Medicine and General Pediatrics, Family Medicine, Psychiatry, General Surgery, Obstetrics, Oncology, Hematology, and, finally, the final rotation block is done in the Microbiology laboratory. These blocks are also essential to an education in Medical Microbiology because they will provide residents with the information needed to be successful on examinations that allow them to continue pursuing their residency program
- From second to fourth year, residents will complete their core microbiology training which consists of topics including bacteriology, virology, mycology, and infection control / antimicrobial stewardship
- Residents spend year five completing rotations in microbiology and participating in added electives that suit intended career paths

Subspecialty Options: Forensic Pathology
Forensic Pathology, often referred to as where medicine and law intersect, is a medical subspecialty of Anatomic and General Pathology that uses laboratory techniques and the study of morphologic and molecular aspects of disease to determine the cause and manner of injury and/or sudden/unexpected death. Forensic Pathologists are responsible for performing autopsies that allow for the laboratory examination of tissue and bodily substances, determining the circumstances surrounding death, interpreting results of post-mortem analyses, providing unbiased opinions based on the findings of medico-legal investigations, and providing their expertise to coroners, law enforcement personnel, judges, lawyers, and other physicians in clinical or legal settings. Dr. Maggie Bellis, a forensic pathologist, describes the favorite thing about her career as its “element[s] of surprise, discovery, detective work, and sometimes of shock!”
To become certified in Forensic Pathology, an accredited residency or fellowship program must be pursued upon completion of an Anatomical or General Pathology residency. In Ontario, there is only one residency program such as this, and it is offered by the University of Toronto
Fact: Although there are many, Forensic Pathology is the only field recognized as a medical subspecialty of, specifically, pathology by the Royal College of Physicians and Surgeons of Canada. Other fields in pathology that are not officially recognized such as Dermatopathology, Cardiovascular Pathology, Surgical Pathology, and Pediatric Pathology are usually pursued through Fellowship Programs offered by universities and institutions. For example Western University offers a 1-year Surgical Pathology Fellowship Program and the University of Toronto does the same with a Genitourinary Pathology Fellowship Program. However, these types of fellowships are pursued after completing a residency program in the field of pathology.
Options for Areas of Focused Competence: Cytopathology and Transfusion Medicine
Firstly, Cytopathology is the Area of Focused Competence within Anatomical or General Pathology that focuses on the examination of any cells and tissue micro-fragments that demonstrate aspects of disease. This examination is done to make/confirm the diagnoses of other physicians, guiding their treatment plan. However, Cytopathology is not the same as the surgical pathological aspects of Anatomical or General Pathology since the preparation and presentation of samples differ. Cytopathologists are responsible for identifying subtle cellular features to distinguish malignant from benign, performing fine needle aspirations to collect diagnostic tissue, interpreting cytological specimens, and managing the cytopathology laboratory. On any given day, these pathologists might diagnose a malignant lung tumor, a woman’s breast carcinoma, or a benign salivary gland mass.
To become certified in Cytopathology, an accredited training program must be pursued upon completion of an Anatomical or General Pathology residency. In Ontario, there are two programs such as this, and they are offered by the University of Toronto and Western University.
Secondly, Transfusion Medicine is the Area of Focused Competence within Hematological and General Pathology that is concerned with providing patients with blood and its components to prevent disease. However, it also focuses on the aspects of the collection, testing, preparation, storage, transportation, and safety of human blood components and their alternatives. Transfusion Medicine Pathologists are responsible for the diagnostic and therapeutic properties of concepts in molecular biology/biotechnology such as immunohematology, apheresis, and histocompatibility; managing the medical laboratory and blood supply; ensuring that blood is being used appropriately; supervising the provision of cell therapy products and human tissues for transplantation; and more. Procedures within the field include testing for blood types and antibodies to determine suitable blood products for patients, determining the cause of transfusion reactions, as well as collecting and transplanting stem cells.
To become certified in Transfusion Medicine, an accredited training program must be pursued upon completion of a General Pathology, Internal Medicine, Hematology, Pediatrics, Hematological Pathology, or Anesthesiology residency. In Ontario, there are two programs such as this, and they are offered by McMaster University and the University of Toronto.

Pros and Cons of Becoming a Pathologist:
Some of the pros of becoming a pathologist include its high salary, with the average salary for a pathologist in Canada being $312,000; its career variety of five medical specialties, which are described above, its convenient working hours and work-life balance, since their work is not usually urgent; and the profession’s demand, as the job outlook for pathologists in Ontario is described as good. Additional pros include the fact that you can work as part of a laboratory team and that the job is compatible with additional roles such as research, management, and teaching.
Some of the career’s cons include the fact that becoming a fully-certified pathologist in one of its branches is a very long process, involving over 10 years of schooling after obtaining a Bachelor’s Degree; that it is an extremely competitive area of medicine, evidenced by the enrolment quotas in place by residency programs; and that it can be a stressful and high-pressure field. Finally, if considering a career in pathology, it is important to understand that they often work without patient interaction; they do most of their work in labs, behind the scenes. Even so, their contributions to patient care are a vital part of the diagnostic process as well as our understanding of disease.
Now understanding the details of what being a pathologist entails, is pathology the right career for you? Wait — don’t answer that yet! First, with your new knowledge of pathology, consider the aspects of a career in medicine that are important to you along with your scientific interests. Next, think about your motivations for becoming a physician and what you see yourself doing in the future. Finally, consider your sense of curiosity’s strength and identify whether it is intrinsic to your personality because, after all, curiosity is what pathology is all about. Now, you can answer the question: Do you want to be a pathologist? Stay tuned for next week’s “So You Want To Be” post!
About the Writer: Hassan is a grade 10 student from Brampton, ON who is passionate about writing and STEM. With a strong commitment to helping others, he plans to pursue a career in medicine, specifically general surgery, and enjoys participating in activities related to the field. An interesting fact about him is that he aims to be fluent in French by the time he graduates high school. In his free time, you can expect to find him reading, planning his day, volunteering, or binge-watching The Office.
